Unraveling the Complexities of Cancer: A Beginner's Guide for Aspiring Medical Students
Introduction
Cancer affects millions of people each year, making it one of the top causes of death worldwide. As a medical student, you’ll soon discover that cancer is not just a single disease but a multifaceted puzzle that requires a deep understanding of its causes, progression, and treatment options. In this beginner’s guide, we’ll cover the fundamentals of cancer, from its development and risk factors to diagnosis, staging, and treatment options. We’ll also explore the importance of supportive care and survivorship and glimpse the future of cancer research. By the end of this article, you’ll have a solid foundation in cancer biology.
What Is Cancer?
Cancer is a pathological state in which aberrant cells multiply unrestricted and form masses or tumors. These tumors disrupt the normal function of organs and tissues in the body.
To understand cancer, you must grasp the basics of cell biology. In a healthy body, cells divide and reproduce under strict instructions encoded in their DNA. However, if genes responsible for regulating cell growth and division acquire specific mutations, cells multiply without restraint, ultimately leading to cancer.
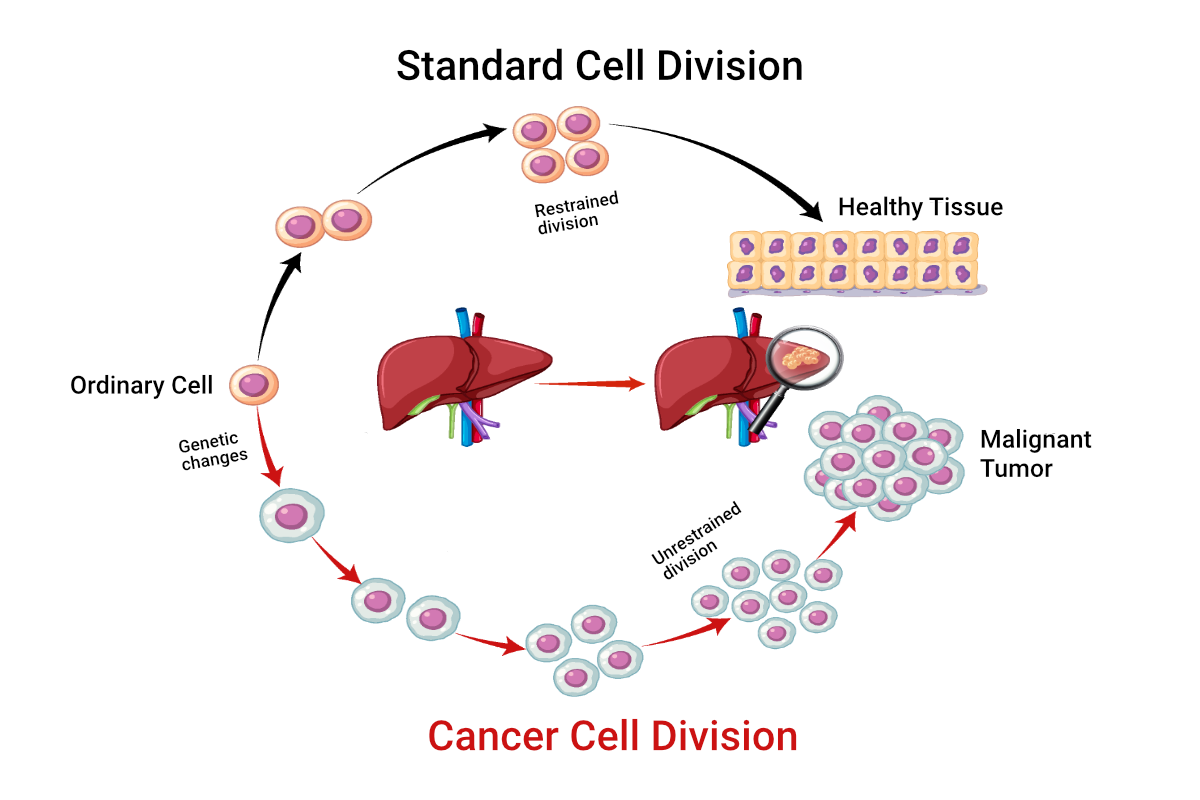
The difference between standard cell division and cancer cell division
Cancers are of multiple types, each named after the tissue or organ where it starts. For example, blood cancer begins in the blood, colon cancer begins in the colon, and brain cancer starts in brain tissue.
In the following sections, we will delve into the various aspects of cancer in greater detail. Specifically, we will cover the following topics:
- Cancer Development and Progression
- Risk Factors and Prevention
- Diagnosis and Staging
- Treatment Options for Cancer Patients
- Supportive Care and Survivorship
- Future Directions in Cancer Research
Cancer Development and Progression
Cancer development is a multi-step process that involves the accumulation of genetic mutations over time. Various factors can lead to these mutations, such as exposure to cancer-causing substances, viral infections, and inherited genetic predispositions.
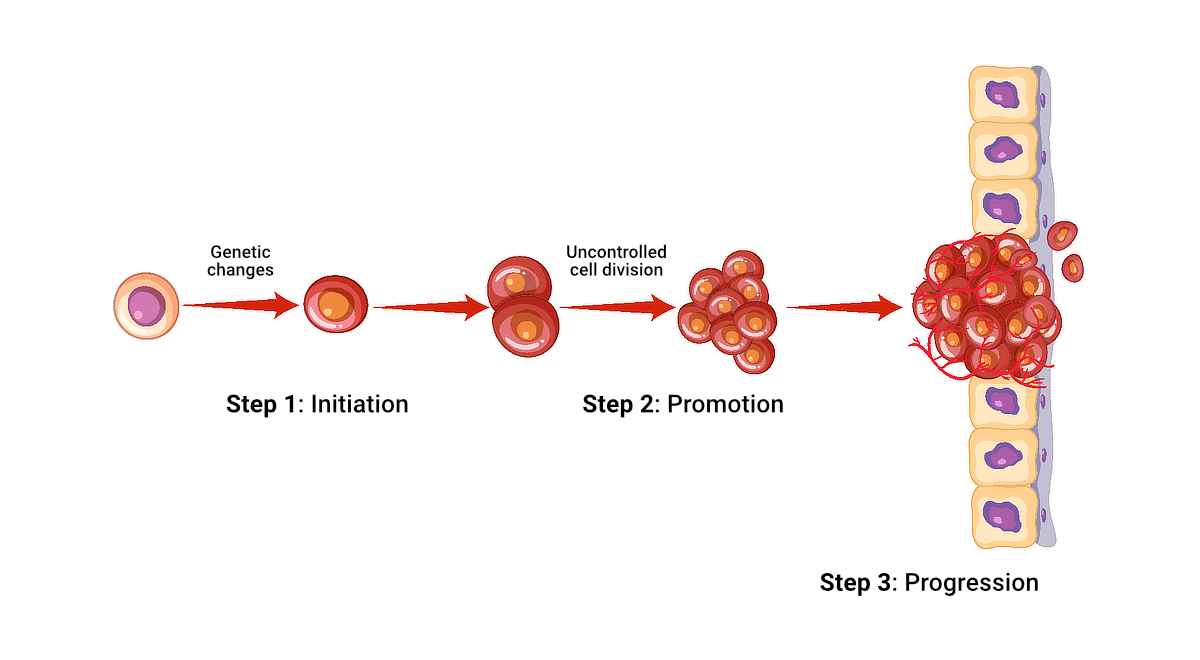
The three-step process of cancer development
The typical progression of a normal cell into a cancerous mass involves the following steps:
- Initiation: A normal cell sustains damage to its DNA, leading to a mutation that alters the cell’s growth and division patterns.
- Promotion: The mutated cell divides uncontrollably, forming a small cluster of abnormal cells.
- Progression: The progression stage marks a critical point in cancer development because it signifies the transition from a benign abnormality to a potentially life-threatening disease. As the abnormal cells grow and accumulate additional mutations, they become aggressive and invasive, eventually transforming into a tumor classified as malignant (cancerous).
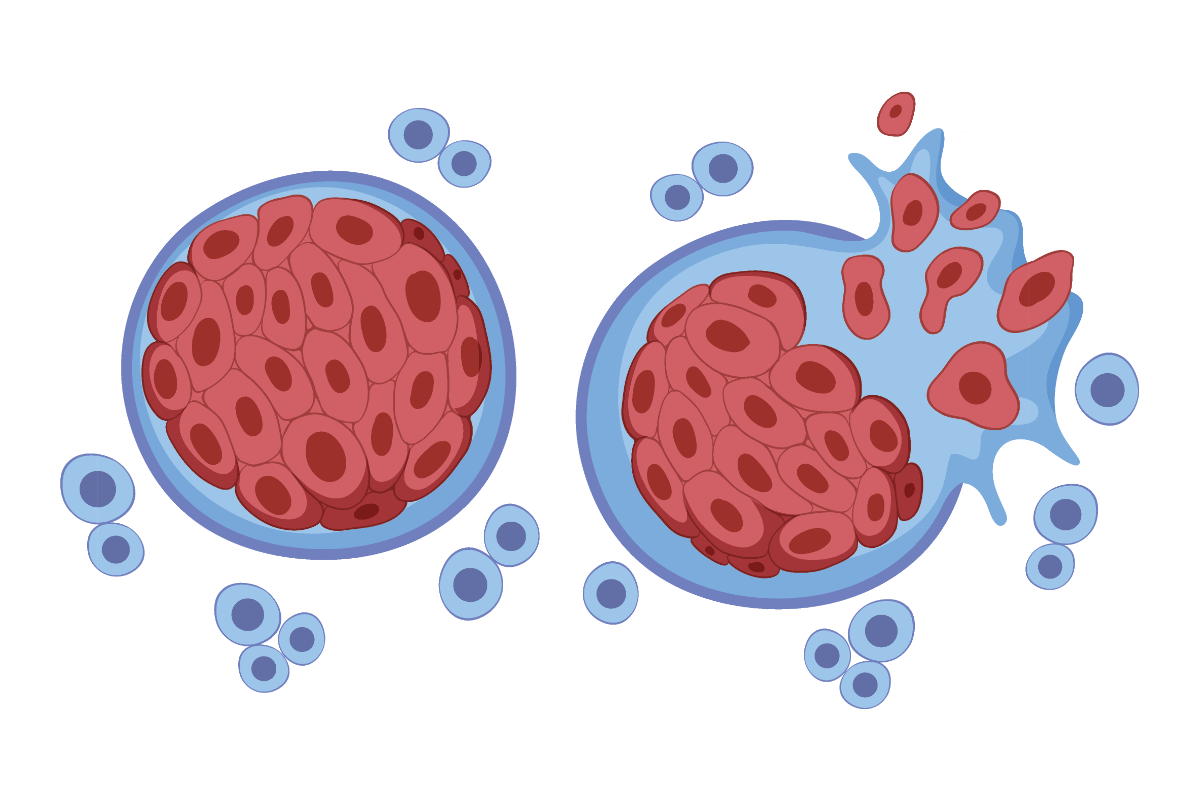
Cancer cells breaking away from a malignant tumor
Once a malignant tumor forms, it has the potential to grow in size. Its cancer cells can also metastasize—undergo metastasis.
During metastasis, breakaway cells from the malignant tumor, which you can now call the primary tumor, move through the lymphatic system or the bloodstream to other organs or tissues. These cells can form new tumors in their new locations.
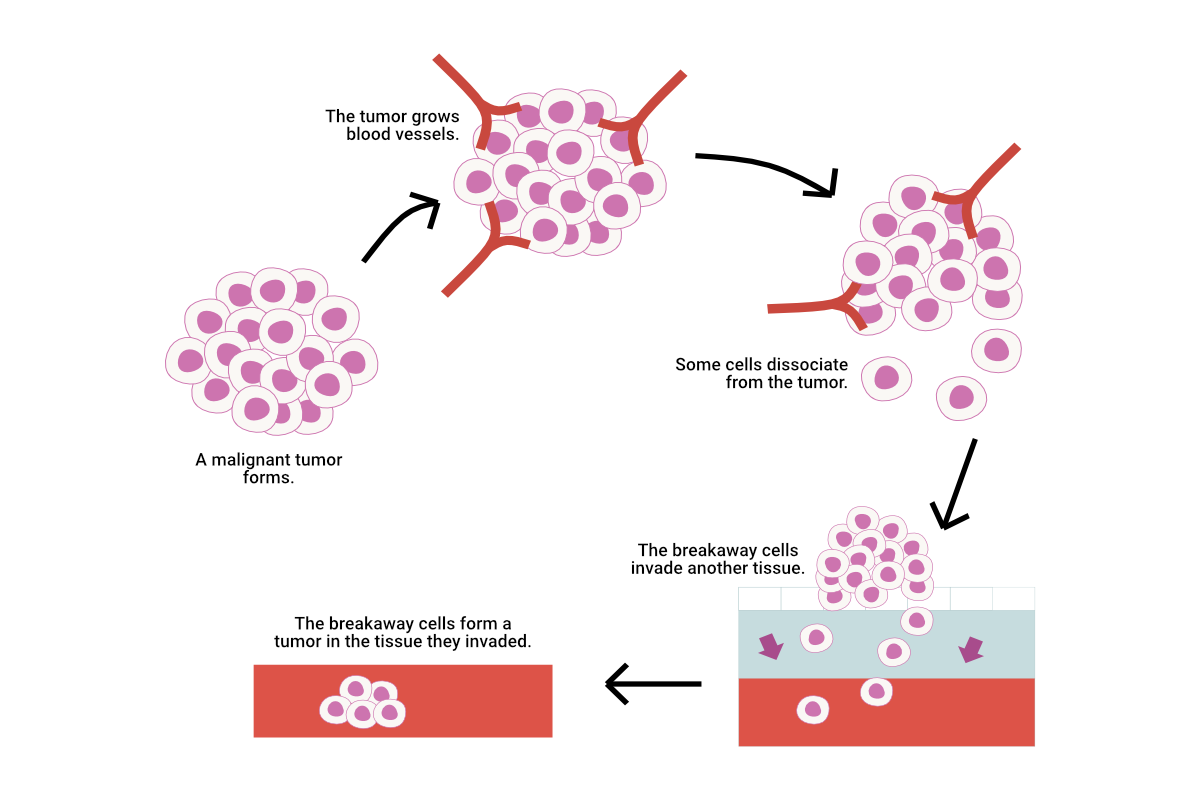
An illustration showcasing the process of metastasis, where cancerous cells dissociate from the primary tumor and form a new tumor in a different location in the body
Metastasis is a life-threatening condition that makes cancer more challenging to treat. Therefore, early detection and treatment of cancer are crucial to prevent metastasis.
Now that you understand cancer development and progression, explore the risk factors associated with cancer in the next section. This section also describes the preventive measures people can take to reduce their cancer risk.
Risk Factors and Prevention
Although the exact reasons behind numerous cancers are still uncertain, scientists have recognized various factors that can heighten an individual’s chances of developing the illness. You can divide these cancer risk factors into two categories: modifiable and unmodifiable.
Modifiable risk factors for cancer include:
- Tobacco use
- Unhealthy diet
- Physical inactivity
- Excessive alcohol consumption
- Exposure to UV radiation (for example, from the sun or tanning beds)
- Exposure to certain chemicals and toxins
Unmodifiable risk factors include:
- Age (the risk of many cancers increases with age)
- Family history of cancer
- Inherited genetic mutations
Understanding these factors is crucial for both prevention and early detection. The table below provides insights into each risk factor, highlighting prevention strategies for modifiable risks and offering context for unmodifiable risks.
Table 1: Detailed Overview of Cancer Risk Factors and Prevention Strategies
| Risk Factor | Description and Prevention Strategies |
|---|---|
| Tobacco use | Major cancer risk; avoiding tobacco use can significantly reduce risk |
| Unhealthy diet | Diets low in fruits and vegetables increase risk; a balanced diet can reduce this risk |
| Physical inactivity | Linked to higher cancer risk; regular physical activity reduces this risk |
| Excessive alcohol consumption | Increases risk of several cancers; limiting intake can help reduce risk |
| UV radiation exposure | Leads to skin cancer; protective measures like sunscreen can prevent skin cancer |
| Chemical and toxin exposure | Certain occupational/environmental exposures increase risk; minimizing exposure is preventive |
| Age | Cancer risk increases with age; regular screening can ensure early detection |
| Family history of cancer | Genetic predisposition may increase risk; genetic counseling and testing can help to identify appropriate prevention measures |
| Inherited genetic mutations | Specific mutations significantly increase risk; personalized monitoring and prevention strategies help |
A healthy lifestyle can help people mitigate the risk of cancer. We must maintain healthy daily routines, such as consuming well-balanced diets, engaging in regular physical activities, and refraining from smoking or excessive drinking. Regular check-ups and vaccinations should also be part of our anti-cancer strategy.
Specifically, vaccinations against human papillomavirus (HPV) and hepatitis B can help prevent cervical and liver cancers. Regular screenings like mammograms and colonoscopies play a crucial role in detecting breast and colorectal cancer early on when treatment is most successful.
Read about Gillian, who faced an unmodifiable risk. Her story illustrates how prevention strategies and regular screenings can help us maintain good health.
Gillian’s Journey: Triumph Over Breast Cancer

Gillian is cancer-free now.
Gillian, a 50-year-old high school teacher, embodies the triumph of proactive cancer prevention and early detection. Understanding the critical role of regular screenings, especially considering her family history of breast cancer, Gillian has been diligently attending her annual mammogram for the past 10 years. She also maintains a healthy lifestyle and avoids tobacco and alcohol.
This year, her screening revealed a small, early-stage tumor in her breast. Because of the early detection of this tumor, doctors treated Gillian’s cancer with a localized therapy, minimizing damage to surrounding healthy tissue. This therapy led to her swift recovery and an excellent prognosis, which is the likelihood of a patient’s full recovery from cancer.
Following surgery and a course of treatment tailored to her specific condition, Gillian made a full recovery. She credits her survival to her commitment to regular mammograms and her health consciousness.
Gillian’s story highlights the relevance of awareness and prevention measures in the battle against cancer. Inspired by her experience, Gillian now advocates for cancer prevention through lifestyle changes and regular screenings, sharing her story to educate others.
By understanding cancer risk factors and prevention strategies, you are empowered to educate patients about proactive choices, potentially reducing their risk of developing this disease. Knowing how cancer is diagnosed and staged is crucial for guiding patients towards the most effective treatment options and improving their quality of life. Let’s delve into cancer diagnosis and staging next.
Diagnosis and Staging
When a patient shows signs indicative of cancer, healthcare professionals conduct a series of diagnostic tests and procedures to confirm the disease and determine its extent. The main diagnostic tests are described below:
-
Physical examination: A healthcare provider looks for visible cancer signs or symptoms, such as lumps, swelling, or skin changes.
-
Laboratory tests: Technicians analyze the patient’s blood, urine, and other bodily fluids to detect markers that may indicate the presence of cancer.
-
Imaging tests: X-rays, CT scans, MRIs, and PET scans help to identify tumors and assess their size and location.
-
Biopsy: A healthcare professional removes a small sample of suspicious tissue and examines it under a microscope. This procedure confirms the presence of cancer cells and identifies the specific type of cancer.

A laboratory technician is examining a biopsy sample.
If cancer is confirmed, the next crucial step is staging, which involves assessing the severity of the cancer. The staging process categorizes cancer into one of the following stages:
- Stage I: The cancerous growth is small and confined within the organ where it originated.
- Stage II: The cancer has grown, but it has not spread extensively.
- Stage III: The cancer has advanced and may have extended to nearby lymph nodes and tissues.
- Stage IV: The cancer has extended to distant body parts.
These stages are critical for formulating the appropriate treatment plan and evaluating the prognosis.
Healthcare professionals worldwide use the TNM staging system to determine the stages of cancer. The TNM system evaluates the extent and severity of the disease based on three criteria:
- Tumor (T): This criterion measures the size of the primary tumor and assesses its depth of invasion into the affected organ or surrounding tissues.
- Node (N): This criterion determines whether the cancer has spread to nearby lymph nodes and assesses the extent of this spread.
- Metastasis (M): This criterion checks for cancer in distant organs and tissues, a critical factor that classifies the cancer as Stage IV.
The TNM system is essential for planning treatment, estimating prognosis, and determining eligibility for clinical trials. It also facilitates clearer communication about cancer staging among medical teams globally, helping to ensure that each patient receives the most effective and tailored treatment plan.
Now that you understand cancer diagnosis and staging, find out how healthcare teams develop cancer treatment strategies.
Treatment Options for Cancer Patients
The field of cancer treatment is constantly advancing, with ongoing development and refinement of new therapies and approaches. Various factors, including the type and stage of cancer, the patient’s overall health, and their personal choices, contribute to deciding the appropriate treatment. The main types of cancer treatments are as follows:
- Surgery: Removing the tumor and surrounding tissue through surgery is often the first line of treatment for solid tumors.
- Radiation therapy: Radiologists use powerful radiation to reduce cancer cells and tumors.
- Chemotherapy: Drugs that kill rapidly dividing cells, including cancer cells, are administered orally or intravenously during chemotherapy.
- Targeted therapy: Patients undergoing targeted therapy receive drugs designed to target the unique molecular characteristics of their cancer cells. By focusing on these specific traits, the drugs effectively block the growth and spread of the cancer cells.
- Immunotherapy: The goal of immunotherapy is to stimulate or boost the immune system so that it can battle cancer cells. This approach uses agents that either enhance the body’s natural defenses or target specific aspects of cancer cells to improve immune detection and destruction.
Refer to the table below to better understand the action mechanisms and side effects of the cancer treatment options.
Table 2: Comparison of Cancer Treatment Modalities
| Treatment Type | Mechanism of Action | Common Side Effects |
|---|---|---|
| Surgery | Physically removes the tumor from the body | Pain, infection, bleeding, and recovery time |
| Radiation Therapy | Uses powerful energy beams to target and eradicate cancer cells | Skin irritation, fatigue, localized hair loss |
| Chemotherapy | Administers cytotoxic agents that interfere with cell division, primarily affecting rapidly multiplying cells | Nausea, alopecia, heightened susceptibility to infections |
| Targeted Therapy | Employs drugs designed to interact with unique markers on cancer cells, disrupting cellular processes specific to those cells | Dermatological reactions, hepatic complications, general lethargy |
| Immunotherapy | Boosts or manipulates the immune system to fight cancer | Flu-like symptoms, potential auto-immune reactions |
Doctors use a combination of these treatments to achieve the best possible outcome. For example, a patient might undergo surgery to remove a tumor, followed by radiation and chemotherapy to eliminate any remaining cancer cells and minimize the risk of cancer recurrence.
The success story below illustrates the impactful results of combining advanced cancer therapies, showcasing their real-world effectiveness.
Success Story: John’s Victory Over Melanoma
John, a 52-year-old man, was diagnosed with stage III melanoma, a severe form of skin cancer. Following the removal of the primary tumor through surgery, John underwent a combination of targeted therapy and immunotherapy, which was crucial given the aggressive nature of his cancer. The targeted therapy specifically targeted the genetic mutations found in his tumor. The immunotherapy boosted his immune system to fight off any remaining cancer cells.
The result was a complete remission, and now, three years later, John remains cancer-free. He attributes his successful outcome to the advanced treatment options and the personalized care plan developed by his oncology team. This case highlights the importance of combining treatments tailored to the patient’s specific type of cancer and the role of innovative therapies in overcoming advanced disease.
As a future medical professional, staying current with the latest advancements in cancer treatment will help you provide the best possible care to your patients. Next, learn about the importance of supportive care and survivorship in the cancer journey.
Supportive Care and Survivorship

Supportive care helps patients navigate the side effects of treatment and preserve their overall well-being.
Going through cancer treatment can be profoundly challenging, impacting patients both physically and emotionally. Supportive care plays a vital role in helping patients navigate the side effects of treatment and preserve their overall well-being. Supportive care includes a variety of services, such as these:
- Pain management: This service focuses exclusively on alleviating pain associated with cancer and its treatment. It employs various techniques and medications designed to reduce or eliminate pain, directly improving the patient’s comfort. Pain management methods can include pharmaceuticals such as analgesics and opioids, physical therapies, and interventional procedures like nerve blocks, all explicitly aimed at managing pain levels to enhance the patient’s quality of life.
- Nutrition support: This service provides guidance and interventions from dieticians to ensure patients maintain adequate nutrition during treatment. It aims to manage side effects and strengthen immune responses.
- Psychosocial support: This service provides therapeutic counseling and facilitates support groups to help patients and their families cope with the emotional stresses associated with cancer diagnosis and treatment. It provides a crucial emotional buffer.
- Rehabilitation: This service includes therapies aimed at helping patients regain strength, mobility, and functionality that cancer treatment may have compromised.
- Palliative care: This holistic approach provides emotional, social, and spiritual support alongside pain management. It involves a team of professionals from different disciplines who work together to improve the quality of life for patients and their families. This team offers various services, including medical treatment, emotional counseling, and assistance with healthcare decision-making.
While supportive care focuses on addressing the immediate challenges during active treatment, survivorship marks a pivotal transition to ongoing care and recovery. It concentrates on the health and well-being of individuals who have finished cancer treatment.
Survivorship involves the following services:
- Long-term management: Addressing the long-term effects of cancer and its treatment, such as chronic pain, fatigue, and neuropathy, are the hallmarks of this service.
- Continued psychosocial support: As treatment ends, support shifts to help survivors adapt to life after cancer, including counseling and group therapies that foster community and emotional well-being.
- Ongoing rehabilitation and palliative Care: These services play a critical role in the survivorship phase, helping survivors manage persistent symptoms and improve their quality of life as they adjust to life after cancer treatment.
To illustrate the profound impact of comprehensive supportive care and highlight the ongoing journey of survivorship, consider the story of Lisa, a breast cancer survivor.
Beyond Survival: Lisa’s Journey From Cancer Treatment to Thriving in Survivorship
Lisa’s cancer journey was multifaceted. It involved intense treatment phases followed by a critical post-treatment survivorship period.
During her treatment, supportive care helped her manage immediate side effects. Pain management specialists, nutrition support, and psychosocial counselors provided targeted care to mitigate the harsh impacts of her treatment.
As she transitioned to survivorship, Lisa’s care adapted to her evolving needs. Lingering fatigue, neuropathy, and emotional distress became the focus of her supportive care. Rehabilitation efforts intensified to restore her physical strength and mobility, while ongoing psychosocial support helped her process her experiences and connect with other survivors.
Lisa’s successful adaptation to survivorship underscores the importance of continuous supportive care. Her story demonstrates that survivorship is about thriving, not just surviving. It highlights the need for comprehensive care that extends beyond the end of active treatment.
From Lisa’s experience, it is clear that both during-treatment supportive care and focused survivorship attention are crucial for ensuring that individuals not only survive cancer but thrive afterward. This knowledge is vital for medical students and healthcare providers aiming to deliver comprehensive, patient-centered care.
In the next section of this guide, we will explore future directions in cancer research and their potential impact on patient care.
Future Directions in Cancer Research
Cancer research is rapidly evolving, with scientists and medical professionals working tirelessly to develop new treatments, improve early detection methods, and enhance patient outcomes. The following are some of the most promising areas of cancer research:
- Precision medicine: Customizing cancer treatment based on an individual’s unique genetic and molecular profile to enhance treatment efficacy and reduce side effects
- Immunotherapy: Harnessing and enhancing the immune system’s natural ability to fight cancer
- Liquid biopsies: Using blood samples to detect cancer cells or DNA fragments, which allows for less invasive, more frequent monitoring of cancer progression or response to treatment
- Cancer vaccines: Developing vaccines to prevent or treat cancer by stimulating the body’s immune response against cancer cells
- Artificial intelligence techniques: Applying advanced computational methods to analyze large datasets, which can lead to the discovery of new drug targets or optimize treatment protocols

Cancer researchers discussing a breakthrough
As a future medical professional, you must remain up to speed with the latest advancements in cancer research. By understanding the potential impact of these developments, you can help guide your patients through the rapidly changing landscape of cancer care and offer them hope for a better future.
Conclusion
In this beginner’s guide, we’ve explored the fundamentals of cancer, from its development and risk factors to diagnosis, staging, and treatment options. We’ve also discussed the importance of supportive care and survivorship and gauged the future of cancer research.
As a first-year medical student, the knowledge you have acquired from this guide will form a firm foundation for your future studies and clinical practice. However, it’s important to remember that cancer is a complex and ever-evolving field; there will always be more to learn.
As you progress through your medical education and training, you’ll have the opportunity to deepen your understanding of cancer biology, explore new treatment approaches, and contribute to the ongoing fight against this devastating disease. By staying curious, compassionate, and committed to lifelong learning, you can make a meaningful difference in the lives of those affected by cancer.
So, take the knowledge you’ve gained from this guide and use it as a springboard for further exploration and discovery. The world of cancer medicine offers challenges and opportunities. As a future medical professional, you have the power to shape its future and improve the lives of countless patients along the way.

